Varicose Veins: Understanding, Management, and Treatment
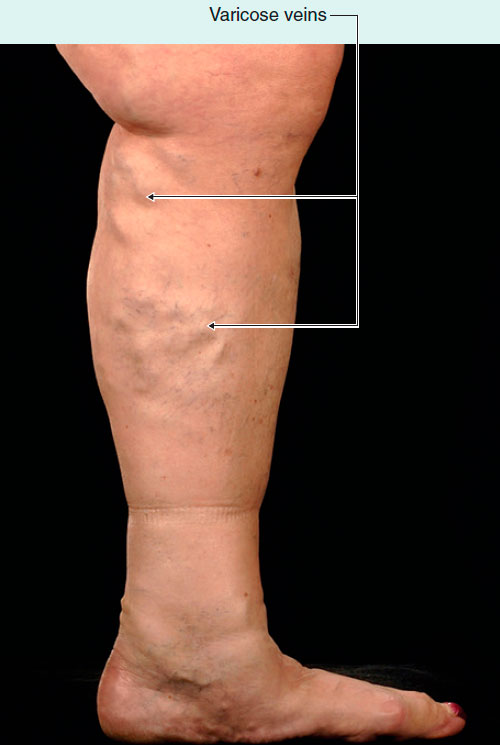
Varicose veins, a widespread vascular disorder, are characterized by tortuously enlarged veins often found in the legs, though they can also occur in the superficial veins of the arm and other organs. These veins, large and twisted, result from weakened or damaged vein walls and valves, causing not only cosmetic concerns but also potential complications impacting the quality of life.

Varicose Veins
The Physiology of Vein Function and the Development of Varicose Veins
Understanding the pathophysiology of varicose veins necessitates a basic grasp of the physiology of vein function. In healthy individuals, the contraction and relaxation of adjacent leg muscles facilitate the pumping of blood from the veins back to the heart. Blood also moves from superficial veins through the investing layer of fascia of the leg into the deeper veins.
However, over time, the valves in these perforating veins may become damaged, leading to a phenomenon known as venous reflux or the backward flow of blood. This reverse flow results in an increase in volume and pressure within the superficial veins, causing them to become dilated and tortuous, the telltale signs of varicose veins.
Consequences of Varicose Veins
Varicose veins, apart from being unsightly, can result in several complications. The skin overlying these enlarged veins may become pigmented and atrophic, showing a poor response to tissue trauma. In some patients, even minor trauma can lead to skin ulceration, necessitating the elevation of the limb and application of pressure bandages to promote healing. Severe cases may also lead to venous ulcers, which require specialized wound care for management.
Causes of Varicose Veins
Varicose veins arise when the walls of the veins weaken. As blood pressure within the vein increases, these weakened walls permit the vein to enlarge. As the vein expands, the valves, which are designed to keep blood moving in one direction within the vein, become less effective. This leads to a sluggish blood flow that backs up or pools within the vein, causing it to swell, bulge, and twist. Several factors can weaken the vein walls and valves, including hormonal changes, the aging process, excess weight, restrictive clothing, and prolonged standing, which increases pressure inside the veins.
Treatment of Varicose Veins
The management of varicose veins is tailored according to their location, size, and severity. For many superficial varicose veins, vein stripping is a common procedure. This surgical method involves the removal of varicose veins, thus redirecting blood flow exclusively into the deep venous system.
However, vein stripping is not the only option for varicose vein treatment. Other treatments may include endovenous laser therapy or radiofrequency ablation, which use heat to close off the varicose veins. Sclerotherapy, another option, involves injecting a solution or foam into the vein to seal it off.
Lifestyle modifications, such as regular exercise, weight loss, and wearing compression stockings, can also help manage the symptoms of varicose veins and prevent new ones from forming.
In conclusion, varicose veins are a common but treatable condition that can significantly impact a person’s quality of life. It is essential to understand their physiology, causes, and available treatment options to manage them effectively. As always, individuals should consult with a healthcare provider to determine the best treatment approach for their specific circumstances.











