Decoding the Mystery of Accessory and Sesamoid Bones
This article provides a comprehensive overview of accessory and sesamoid bones, which can exist as normal skeletal variants in many people. It highlights their common locations in the body – mainly around the wrist, hands, ankles, and feet – and their potential functions. It emphasizes that accessory and sesamoid bones can often be mistaken for fractures in imaging studies, highlighting the need for accurate identification. The article also explores potential pathologies associated with these bones, which can be triggered by trauma, degenerative changes, inflammation, or excessive mechanical stress. Treatment strategies for these pathologies, including conservative management and surgical excision, are also discussed. The information presented in this article underscores the clinical significance of accessory and sesamoid bones in accurate diagnosis, treatment planning, and improving patient outcomes.

Accessory and Sesamoid Bones
In the intricate realm of human anatomy, accessory and sesamoid bones represent intriguing examples of skeletal variations. These structures, though not typically part of the standard skeleton, can occur as normal variants in a significant number of people. A thorough understanding of their potential locations, functions, and associated pathologies can be crucial in medical practice, particularly in differential diagnosis and targeted treatment planning.
Accessory Bones: Unexpected Extras
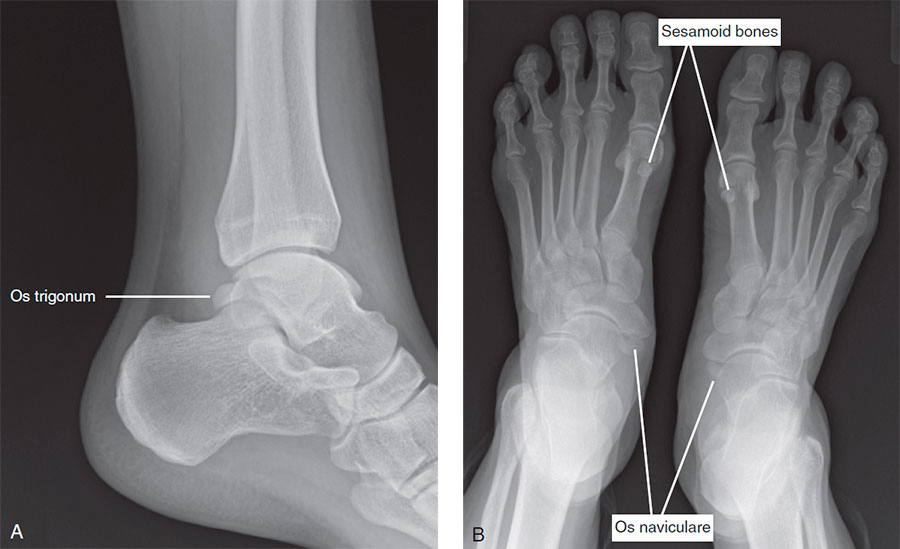
Accessory bones, often discovered incidentally on radiographs or during surgeries, are generally found around the wrist, hands, ankles, and feet. These bones originate from a failure in the fusion of regular ossification centers during embryonic development. As such, they can be mistaken for fractures in imaging studies if not identified correctly. Noteworthy examples include the os peroneum, os trigonum, os acromiale, and os styloideum.
Although accessory bones are usually asymptomatic, complications can arise when these bones are subjected to trauma or excessive mechanical stress. For instance, the os trigonum, found behind the ankle joint, can sometimes cause a painful condition known as os trigonum syndrome. Similarly, an os peroneum fracture can mimic the symptoms of a peroneus longus tendon tear. Therefore, the precise identification of accessory bones can be instrumental in the accurate diagnosis and management of various orthopedic conditions.
Sesamoid Bones: Hidden in the Tendons
Unlike accessory bones, sesamoid bones are embedded within tendons or muscle tissues. The largest and most well-known sesamoid bone is the patella or kneecap, crucial for enhancing the mechanical advantage of the quadriceps tendon. Other sesamoid bones, often smaller, can be found in several locations in the body, particularly within the flexor tendons of the hands and feet, such as the thumb and big toe.
Sesamoid bones serve several functions, including protecting tendons from wear and tear, increasing the mechanical advantage of tendons, and absorbing impact. However, due to their locations, they are often subject to significant mechanical stresses, potentially leading to pathologies like sesamoiditis, osteoarthritis, and fractures.
Managing Accessory and Sesamoid Bone Pathologies
When accessory or sesamoid bones become a source of discomfort or pain due to degenerative changes, inflammation, or mechanical stresses, a range of treatment options can be employed. Initial interventions often include conservative management strategies such as rest, physiotherapy, or targeted steroid injections to reduce inflammation and pain.
However, in severe or refractory cases, surgical removal of the problematic bone, known as accessory or sesamoid bone excision, may be necessary. Although generally safe and effective, as with any surgical procedure, potential complications and patient-specific factors must be considered in the decision-making process.
In conclusion, accessory and sesamoid bones, though often overlooked, hold substantial clinical significance. Awareness and understanding of these bones can greatly assist clinicians in making precise diagnoses, planning targeted treatments, and ultimately improving patient outcomes.











